Soft tissue regeneration
EMPOWERING REGENERATION
Our focus at REGEDENT is to provide solutions to address the cause of the periodontal and peri-implant infection (biofilm) and ensure that the cleaned disinfected site is regenerated to ensure long-term tissue health. Our regenerative solutions empower biology to rebuild the complex fibrous structure around teeth (cementum, PDL, alveolar bone) or around implants while minimizing the patient’s discomfort.
SOFT TISSUE REGENERATION: PERIODONTOLOGY VS IMPLANTOLOGY
Regenerative dentistry has an approach based on understanding the underlying mechanisms of tooth development and the biological processes of healing and repair to leverage the healing potential of the dental tissues [1]. Around the implant, the epithelial attachment is very similar to the one around the tooth by having, for example, the capability to adhere to bio-inert material such as titanium [2, 3, 4].
The big difference between peri-implant and periodontal soft tissues is the alignment of the connective tissue attachment’s collagen fibers. In the periodontium, the PDL cells are organized orthogonally to the tooth root. In contrast, in peri-implant tissue, they run parallel and show a lesser vascularization due to the desmodont’s absence. Around teeth, the vascularization comes from the periosteum and cortical vessels [5]. The periodontium is composed of the gingiva, the underlying connective tissue, the cementum, the alveolar bone, and the periodontal ligament between the cementum and alveolar bone.
PERIODONTAL REGENERATION
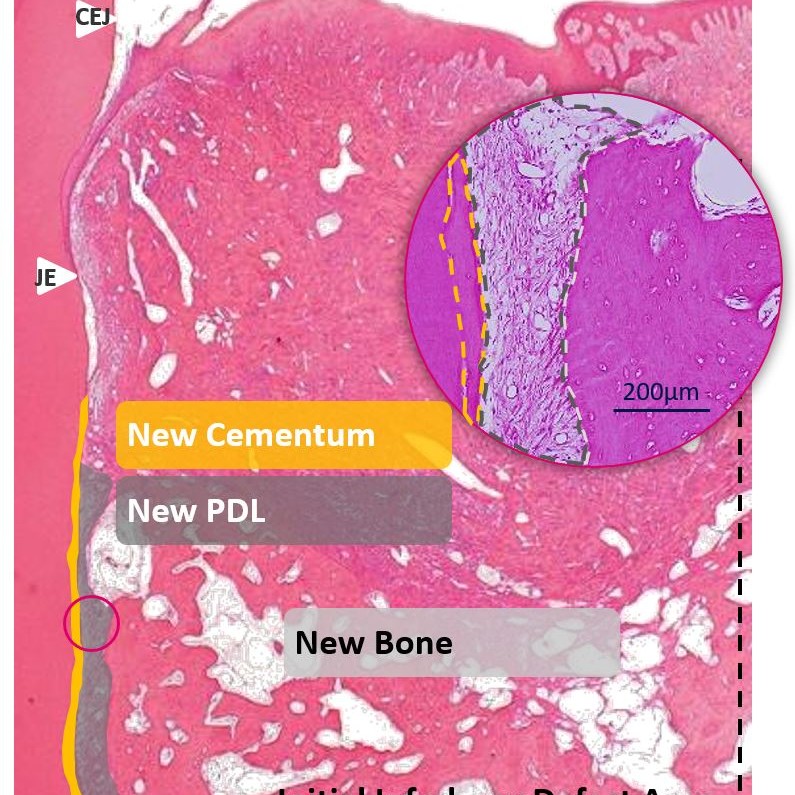
Periodontal disease occurrence is highly prevalent in adult-aged populations worldwide, with prevalence rates around 50% [6]. It is characterized by irreversible damage in the tooth-supporting tissues, including the alveolar bone, periodontal ligament (PDL), and cementum [7]. Traditional therapy is to remove the pathogenic biofilms and suppress the inflammation to stop further periodontal tissue degradation [8]. Poorly controlled periodontal disease leads to infrabony defects, furcation, and potentially and tooth loss [9]. The regeneration of PDL is an essential requirement for periodontal regeneration. The regenerated highly organized collagen fibers play their functional role for tooth health [10].
REGENERATION IN IMPLANTOLOGY
In implantology, the peri-implant soft tissue interface plays an important role in implant-supported restorations’ long-term success [12]. Dental implants do not benefit from the periodontal ligament vasculature, and therefore, the surrounding tissue has a limited blood supply compared to natural teeth [13,14]. Controlling and preventing peri-implant disease limits the risk of soft tissue recession, leading to mucositis or even peri-implantitis.
THE TEN SIGNS OF SUCCESSFUL SOFT TISSUE REGENERATION
- User friendly, cost-effective, predictable treatment protocol
- Rapid blood clot stabilization
- Use of biocompatible material
- Minimize inflammatory process (swelling, discomfort)
- Rapid angiogenesis
- Uneventful wound healing
- Scarless effects for better esthetics
- Avoid infection relapses
- Stable tissue and bone level
- Patient and clinician satisfaction
OUR BIO-ACTIVATOR TO REGENERATE SOFT TISSUE
Hyadent BG is designed to support regeneration [1,2], while being user-friendly. Indeed, the gel can be applied on any tooth surface, with no pre-requisite for prepared and/or dried surfaces [3].
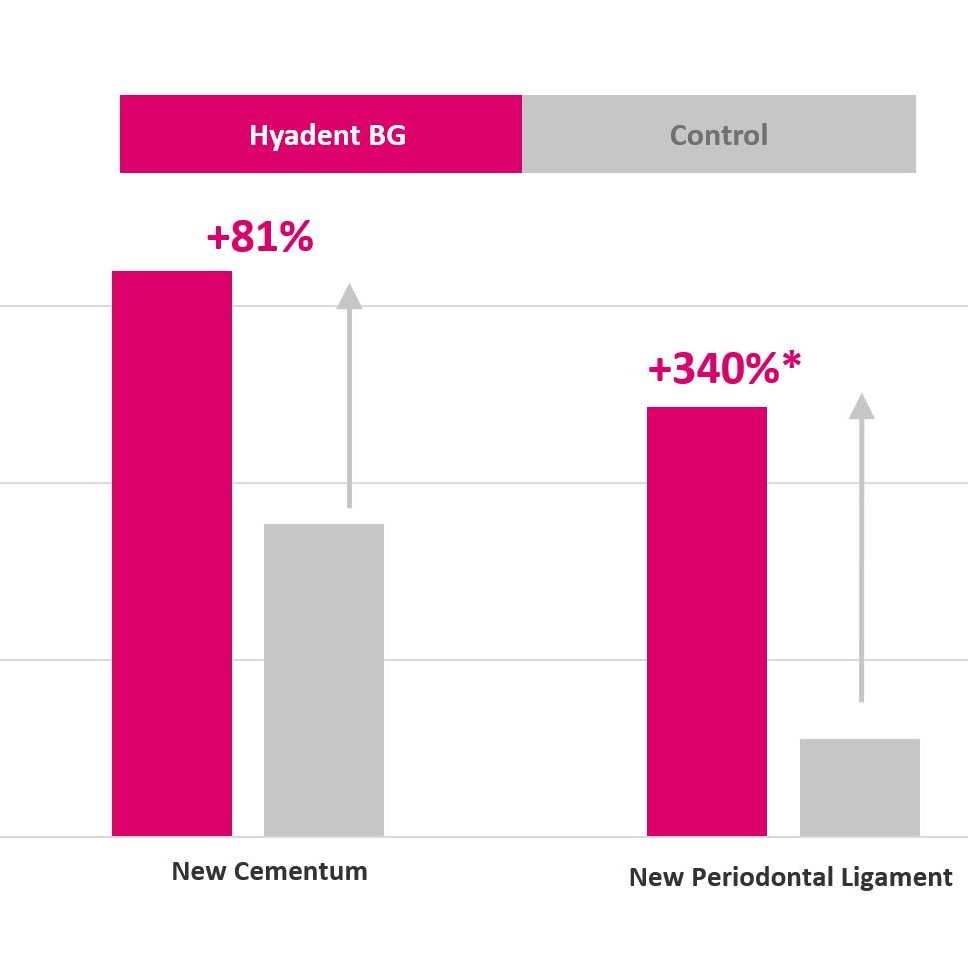
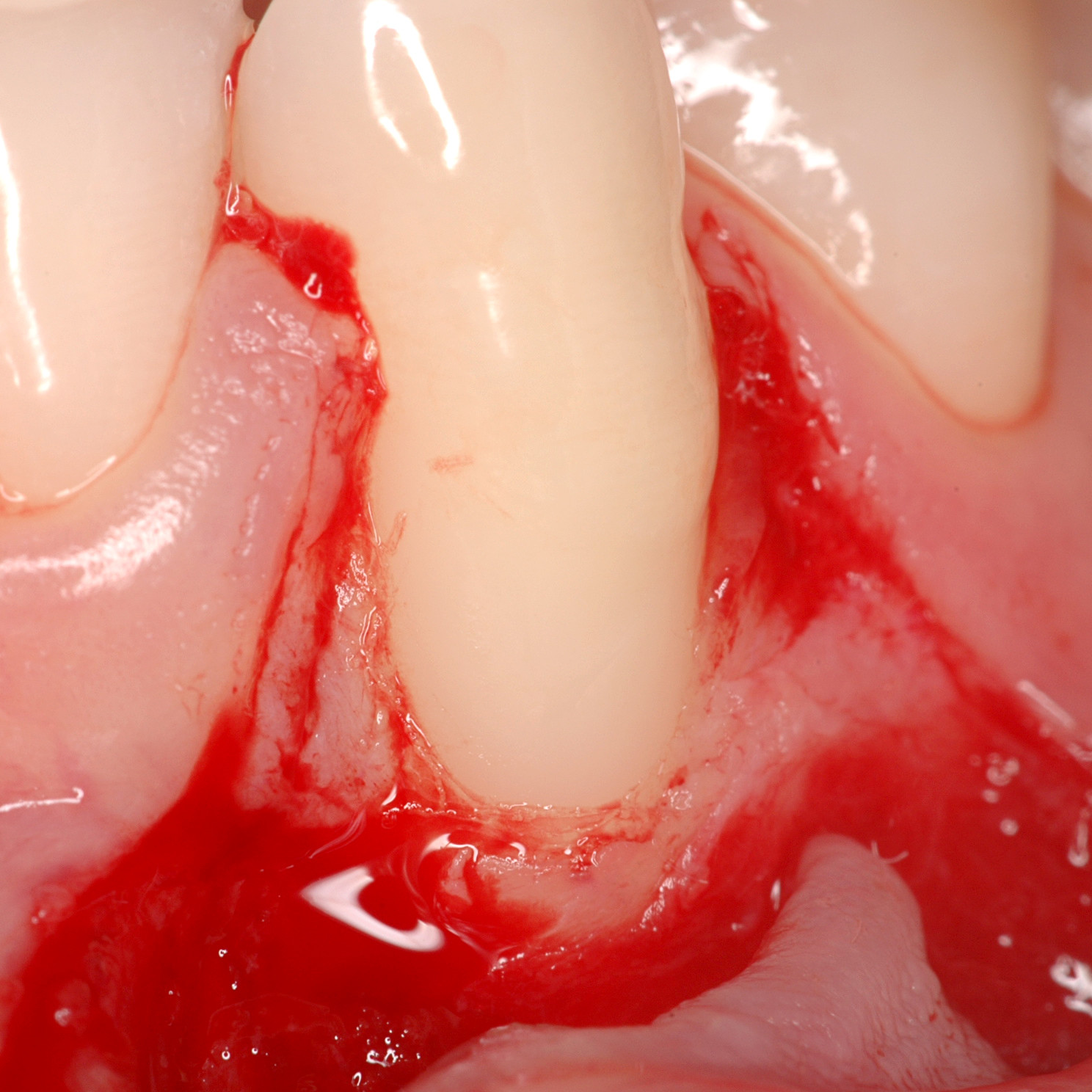
Hyadent BG contributes to stabilizing the blood clot. Its hyaluronic acid attracts the growth factors naturally present in the blood and promotes vascularization. It was shown that Hyadent BG has a significant effect on the proliferation of cementum, periodontal ligament (PDL), and alveolar bone [4-6].
The cross-linking of the hyaluronic acid extends its positive effect on cell proliferation, maintaining the stemness, while its high molecular weight coordinates the inflammatory process (less swelling, discomfort) [7-10].
During the soft tissue healing process, Hyadent BG’s bacteriostatic property contributes to enhancing the predictability of the overall treatment [11-12]. The acceleration of wound closure provides an upside to patients, healthy or at risk [9,11].
By rebuilding not only the esthetic, but also the functional structure around the tooth, Hyadent BG is considered to regenerate rather than repair [1,2,11,13].
To discover more about hard tissue regeneration, see here.
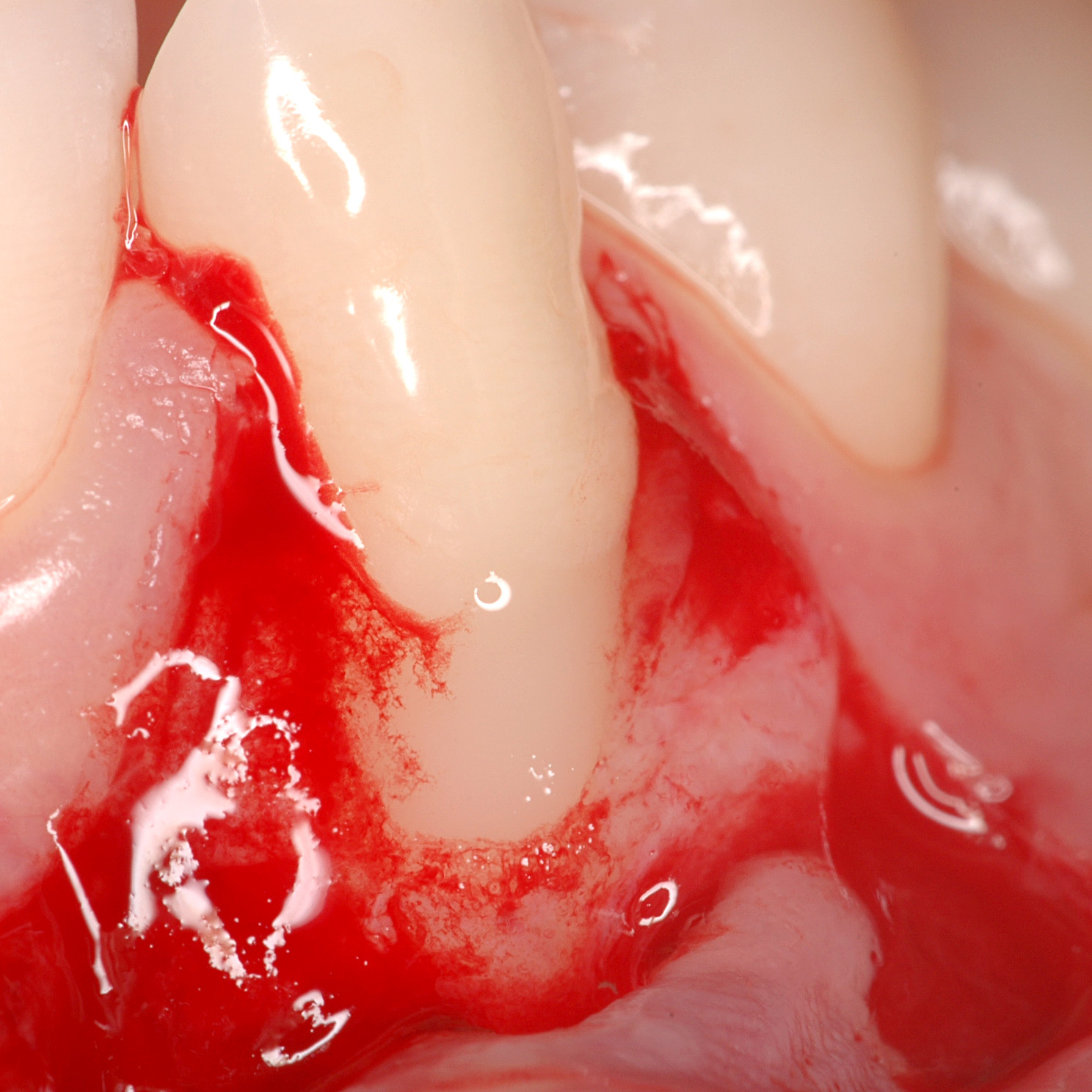
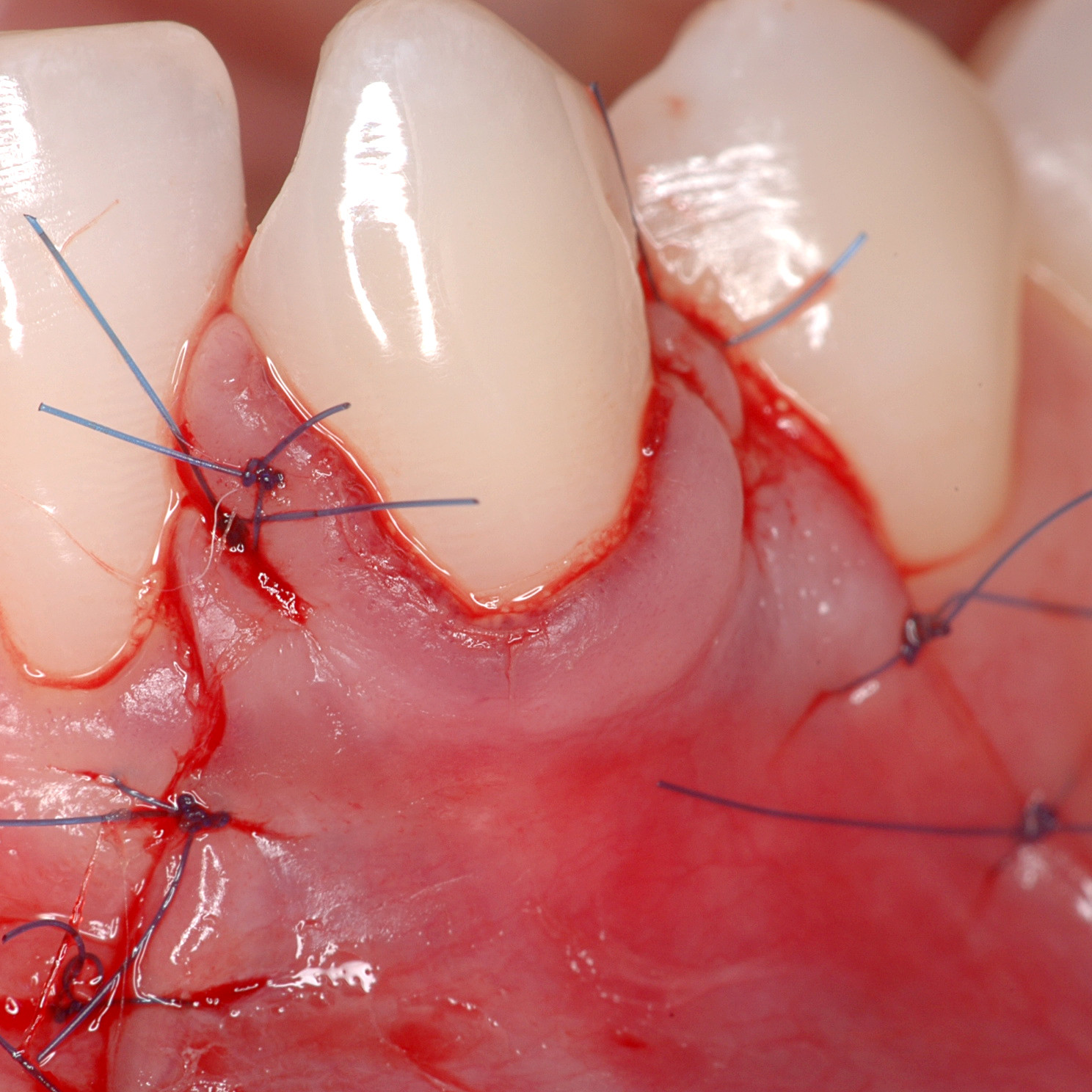
CASE REPORT : SOFT TISSUE REGENERATION IN GINGIVAL RECESSION
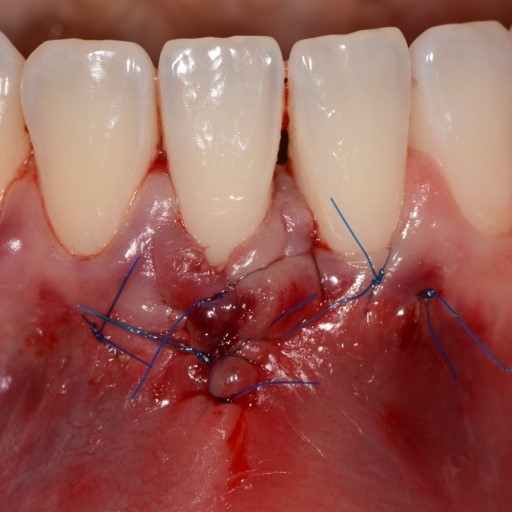
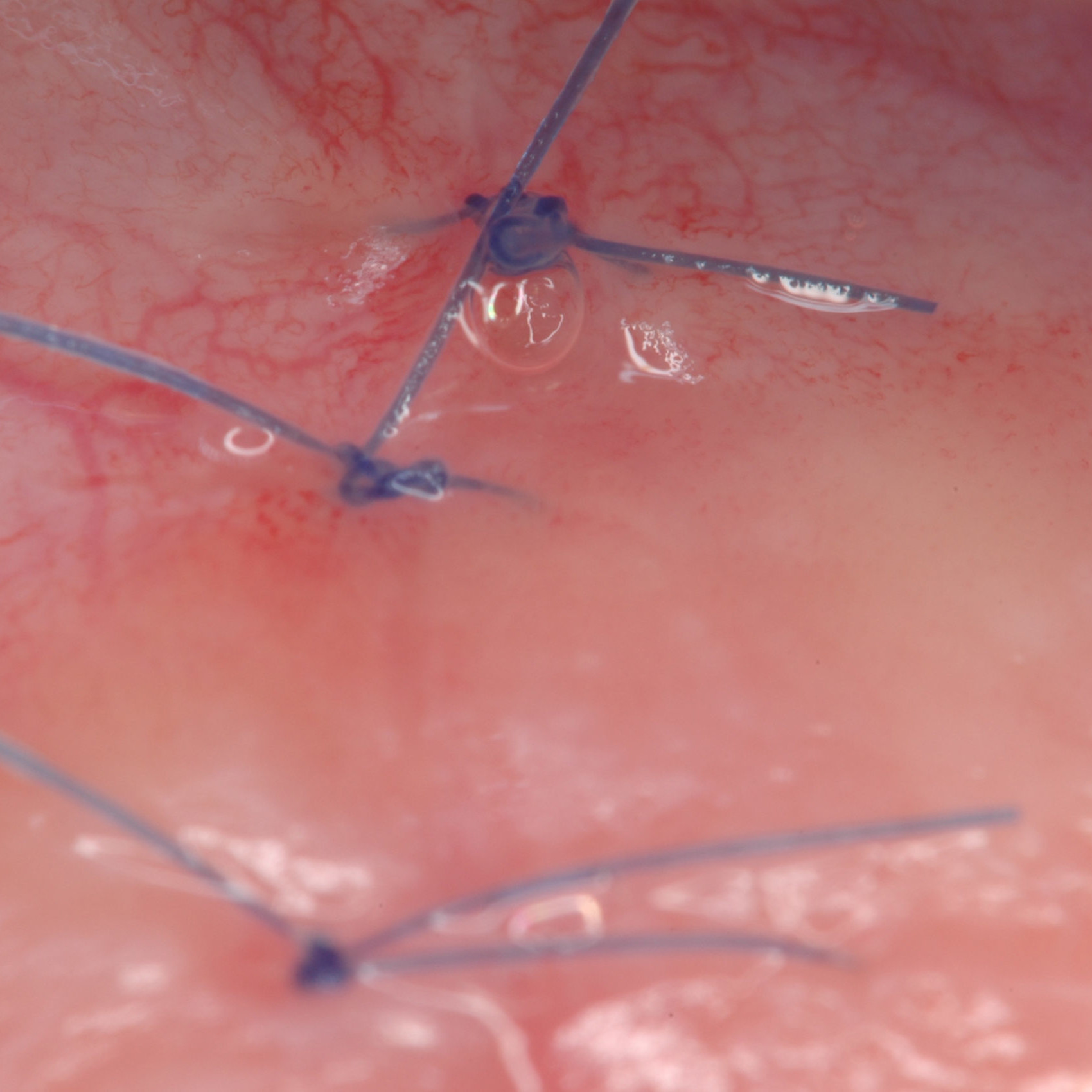
Deep Miller class II recession treated by Prof Anton Sculean with a modified coronally advanced tunnel including conjunctive tissue graft with Hyadent BG
Coronally advanced flap of a gingival recession treated by Prof Andrea Pilloni
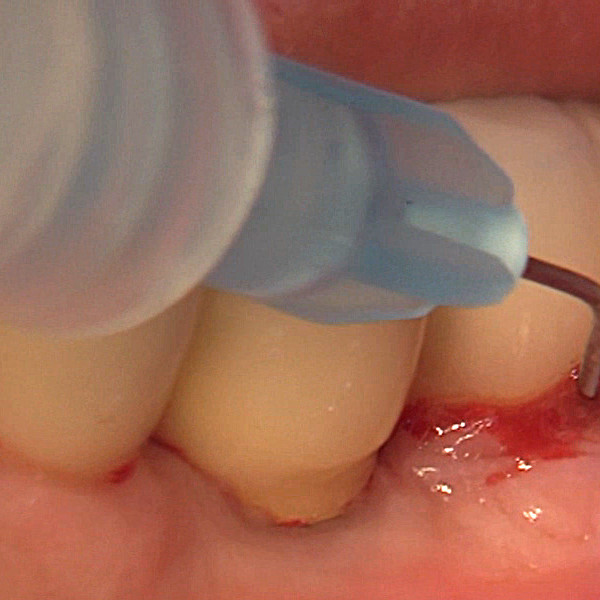
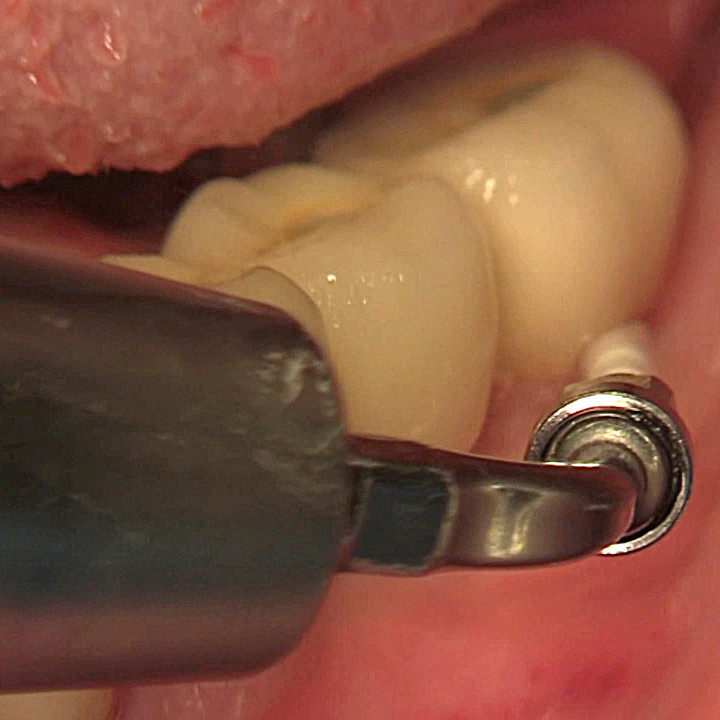
CASE REPORT : SOFT TISSUE REGENERATION IN MUCOSITIS
Mucositis treatment by Dr Marisa Roncati with the Clean & Seal treatment concept
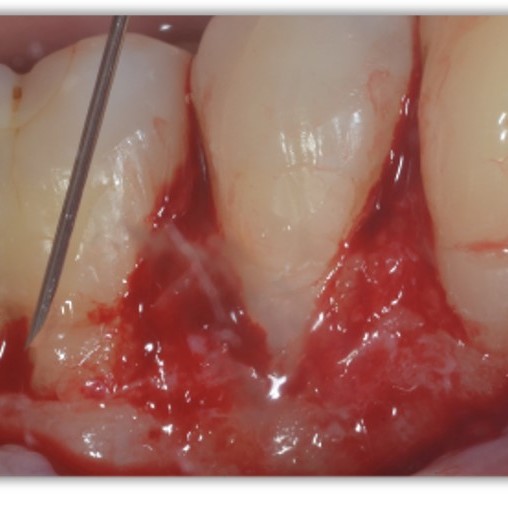
CASE REPORT : SOFT TISSUE REGENERATION IN INTRAOSSEOUS DEFECTS
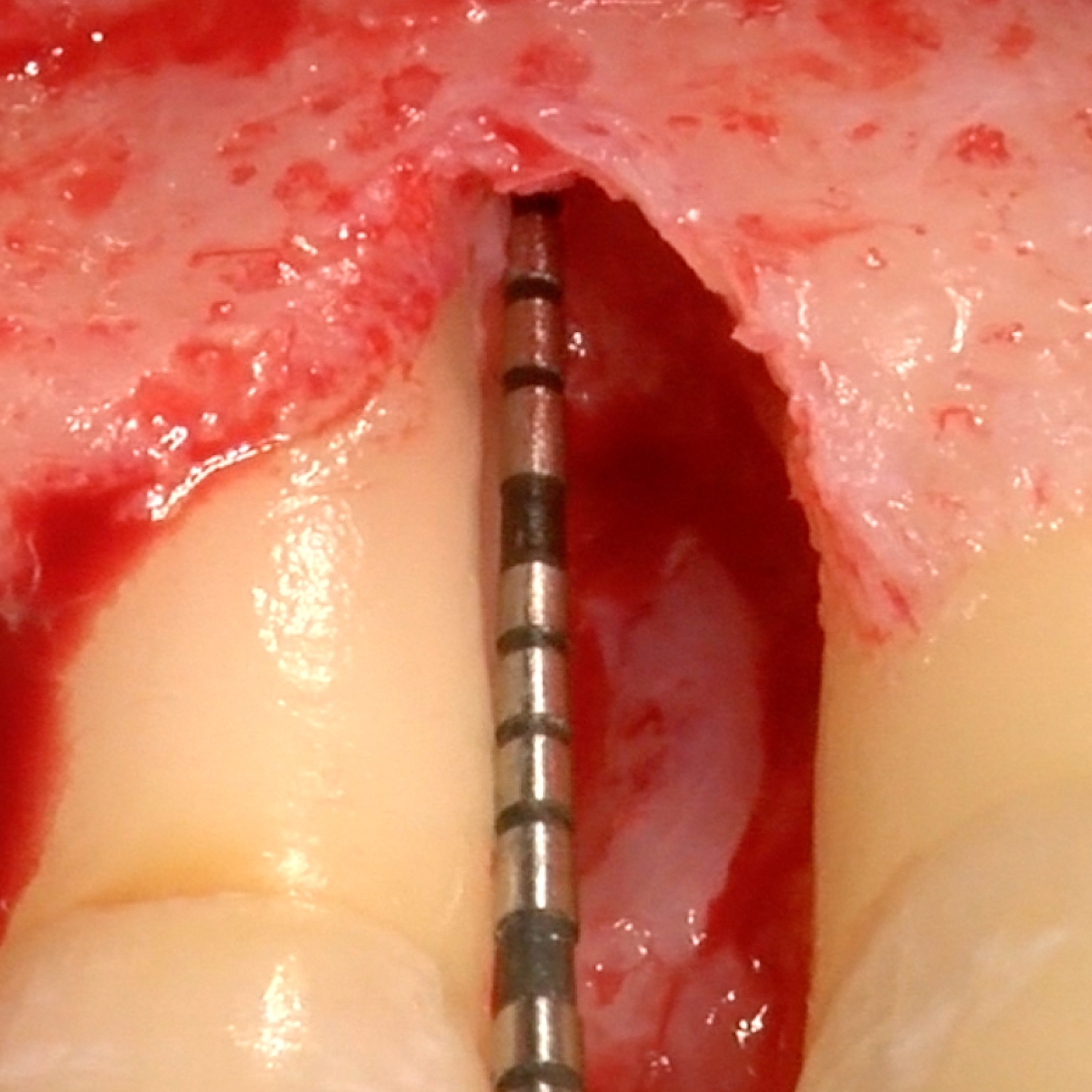
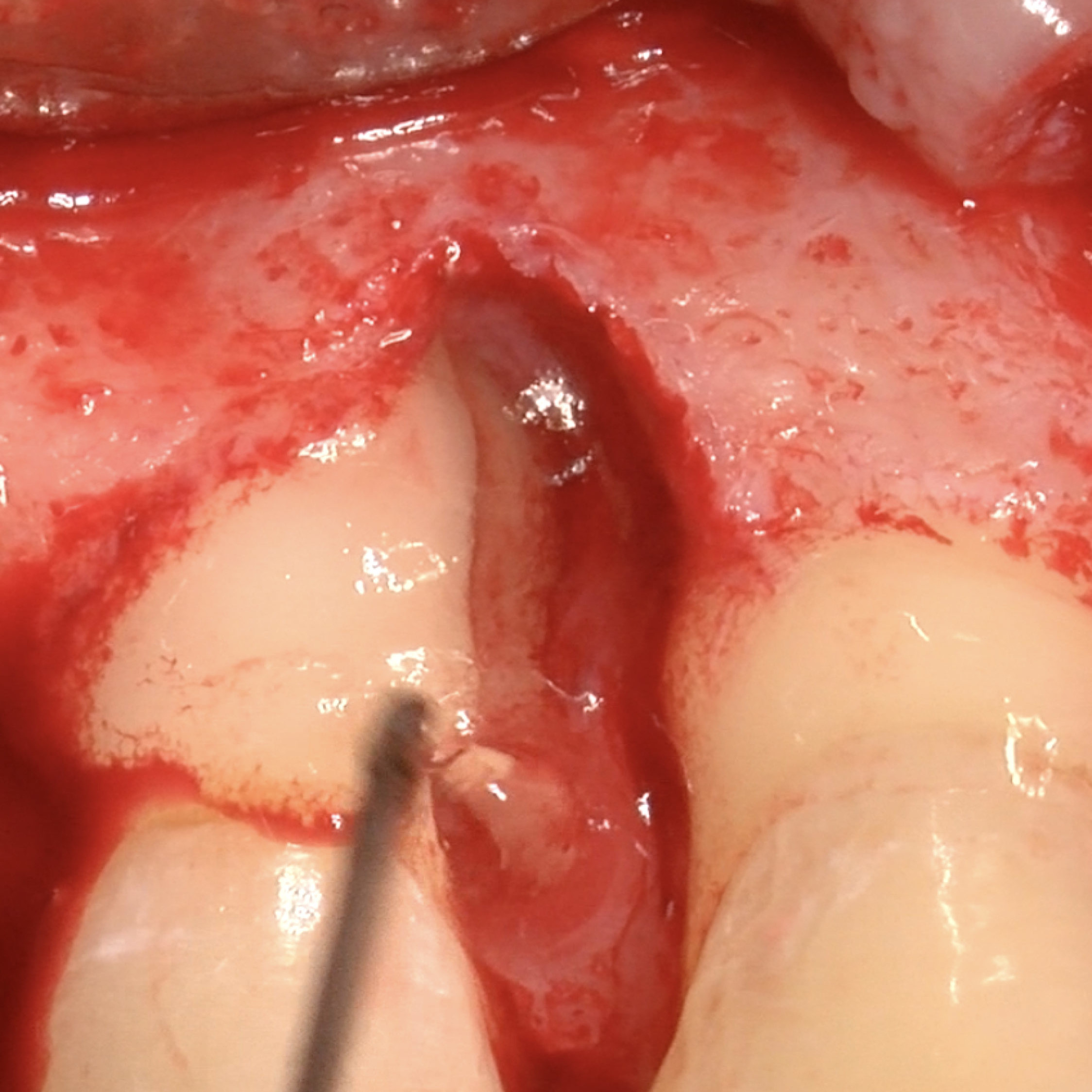
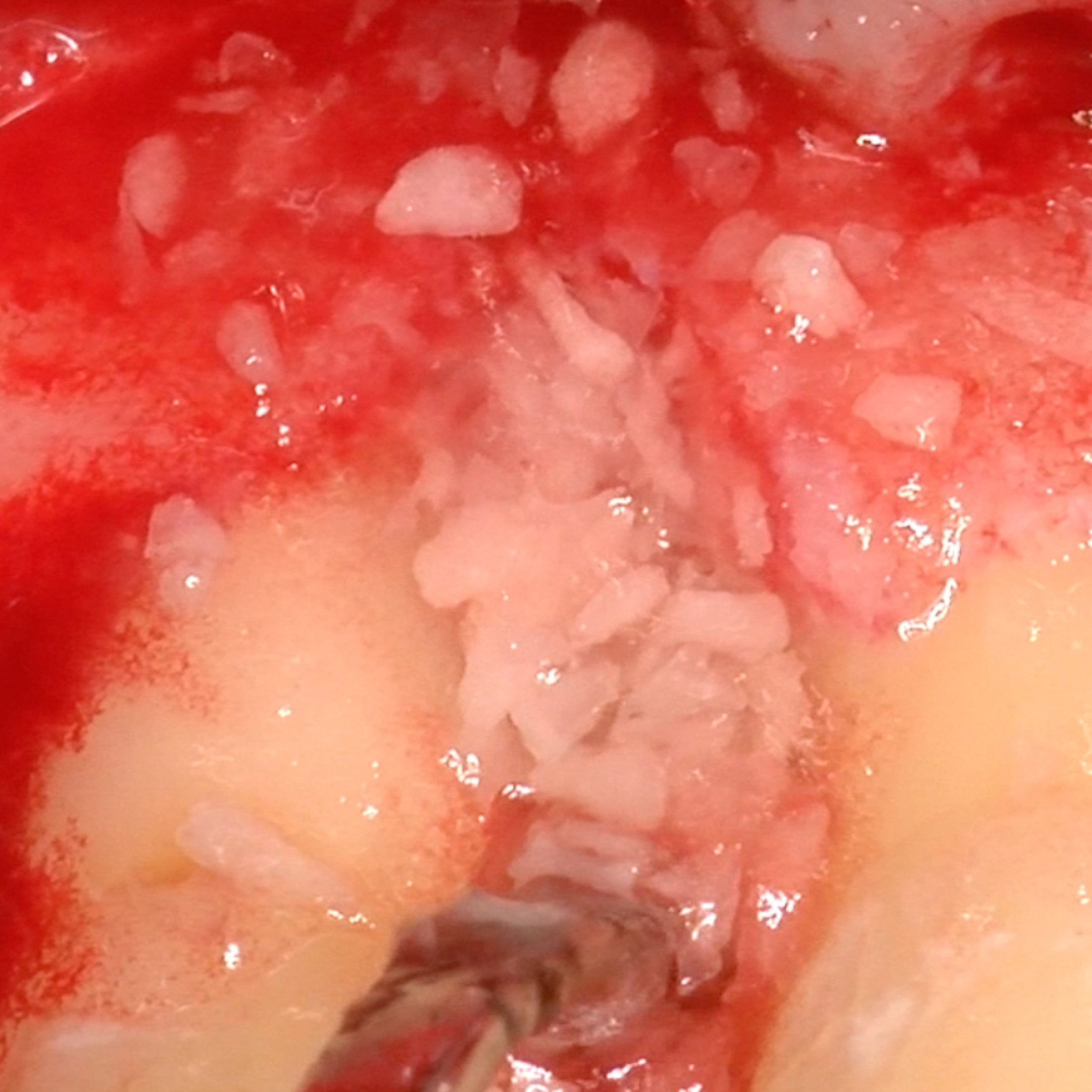
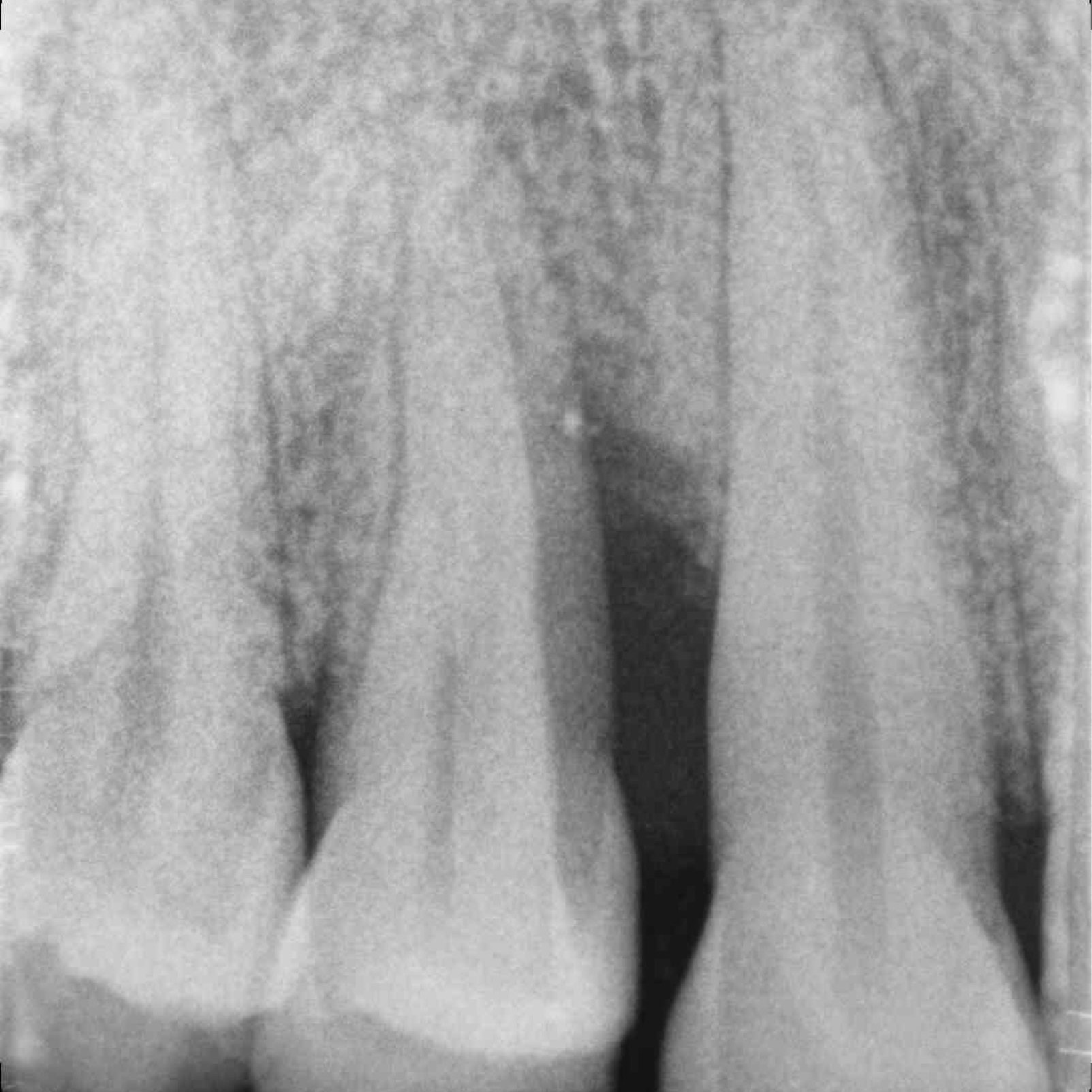
Narrow infrabony defect treated defect by Prof Andrea Pilloni
CLINICAL CASE : SOFT TISSUE REGENERATION IN CASES OF FURCATION
Multiple mandibular recession (RT1) with furcation treated by Dr Sofia Aroca
SCIENTIFIC LITERATURE & CLINICAL STUDIES
- Longaker T et al. ‘Studies in Fetal Wound Healing: V. A prolonged presence of hyaluronic acid characterizes fetal wound healing’ Ann. Surg. 1991; April:292–296.
- Mast BA et al. ‘Hyaluronic Acid Modulates Proliferation, Collagen and Protein Synthesis of Cultured Fetal Fibroblast’ Matrix, 1993;13:441–446.)
- Pilloni A, Rojas M A, Marini L, Paola Russo, Sculean A, Iacono R. Healing of intrabony defects following regenerative surgery by means of single-flap approach in conjunction with either hyaluronic acid or an enamel matrix derivative: a 24-month randomized controlled clinical trial. Clin Oral Invest https://doi.org/10.1007/s00784-021-03822-x
- Fujioka-Kobayashi M, Müller H, Mueller A, Lussi A, Sculean A, Schmidlin PR, Miron RJ ‘In vitro effects of hyaluronic acid on human periodontal ligament cells’ BMC Oral Health (2017) 17:44 DOI 10.1186/s12903-017-0341-1
- Shirakata,Y., Imafuji, T., Nakamura T., Kawakami, Y., Shinohara, Y., Noguchi K., Pilloni, A., Sculean, A.. Periodontal wound healing/regeneration of two-wall intrabony defects following reconstructive surgery with cross-linked hyaluronic acid-gel with or without a collagen matrix: a preclinical study in dogs. An experimental study in dogs. Quintessence Int 2021;52:2-10
- Shirakata Y, Nakamura T, Kawakami Y, et al. Healing of buccal gingival recessions following treatment with coronally advanced flap alone or combined with a cross-linked hyaluronic acid-gel. An experimental study in dogs. Journal of Clinical Periodontology. 2021 Jan. DOI: 10.1111/jcpe.13433.
- Bayoum, A., Nadershah, M., Albandar, A., Alsulaimani, B.S., Sankour, I., Gadi, L., Osama, O.A., Tayeb, R., Quqandi, R., Dabroom, W., & Merdad, Y. (2018). The Effect of Cross-Linked Hyaluronic Acid in Surgical Extraction of Impacted Mandibular Third Molars. International journal of dentistry and oral health, 4.
- Aya KL, Stern R. Hyaluronan in wound healing: rediscovering a major player. Wound Repair Regen. 2014;22(5):579-593. doi:10.1111/wrr.12214
- Kim JJ, Song HY, Ben Amara H, Kyung-Rim K, Koo KT. Hyaluronic Acid Improves Bone Formation in Extraction Sockets With Chronic Pathology: A Pilot Study in Dogs. J Periodontol. 2016;87(7):790-795. doi:10.1902/jop.2016.150707
- Yıldırım S, Özener HÖ, Doğan B, Kuru B. Effect of topically applied hyaluronic acid on pain and palatal epithelial wound healing: An examiner-masked, randomized, controlled clinical trial. J Periodontol. 2018;89(1):36-45. doi:10.1902/jop.2017.170105
- Asparuhova M, Kiryak D, Eliezer M, Mihov D, Sculean A. ‘Activity of two hyaluronan preparations on primary human oral fibroblasts’. J Periodontal Res 2018 Sep 27. Epub 2018 Sep 27
- Eliezer M, Imber JC, Sculean A, Pandis N, Teich S, ‘Hyaluronic acid as adjunctive to non-surgical and surgical periodontal therapy: a systematic review and meta-analysis’, Clin O Inv 2019; doi: s00784-019-03012-w)
- Salbach J et al. ‘Regenerative potential of glycosaminoglycans for skin and bone.’ J Mol Med 2012;90:625–635.